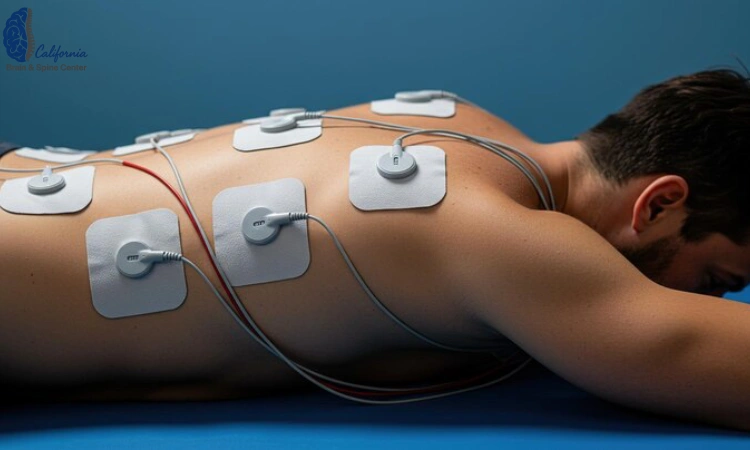
Back Pain Treatment via Electromagnetic Pulse Therapy
Back pain steals more than comfort it steals momentum. If you’ve heard about electromagnetic pulse therapy for back pain and you’re wondering whether it could help you get your life moving again, you’re in the right place. My goal here is simple: explain what it is in plain language, set healthy expectations, and show you a practical, step-by-step way to try it safely while keeping you encouraged every step of the way. You deserve care that’s both hopeful and honest.
What is electromagnetic pulse therapy (PEMF), really?
“PEMF In California” stands for pulsed electromagnetic field. Think of it as gentle, low-energy magnetic waves that are turned on and off in specific patterns. In electromagnetic pulse therapy for back pain, a coil or pad placed near your spine emits these pulses. You don’t feel electricity passing through you; instead, the changing magnetic field induces tiny currents in tissues under the surface. The settings frequency, intensity, and pulse pattern can be adjusted depending on the device and goals.
Unlike heat packs or massage that work mostly at the surface, PEMF attempts to nudge deeper cellular processes. The attraction is obvious: it’s noninvasive, generally comfortable, and it aims to support your body’s natural repair mechanisms rather than “overpower” pain.
Why might electromagnetic pulse therapy help a sore back?

Back pain is rarely just one thing; it’s a conversation between joints, muscles, discs, nerves, and even the way the brain interprets signals. PEMF is not a magic switch, but studies and clinical experience suggest several ways it might help:
-
Cellular energy support: The pulsed field may influence cellular ion channels and mitochondrial activity, which can translate into better tissue recovery signals.
-
Microcirculation: Improved local blood flow supports nutrient delivery and waste removal small gains that can matter when tissues are irritated.
-
Inflammatory balance: After strain or overuse, inflammatory messengers can get “stuck.” PEMF may help nudge that chemistry back toward balance.
-
Muscle tone and guarding: When muscles around the spine clamp down, everything feels worse. Gentle modulation may reduce guarding, making movement easier.
-
Pain signaling: By influencing peripheral nerves and central processing, PEMF can, in some people, reduce the volume on pain without numbing or sedation.
That’s the why behind electromagnetic pulse therapy for back pain: it tries to tip a complex system toward healing not by force, but by tuning.
Low Laser Light Therapy (LLLT) — If you’re weighing non-invasive modalities, we’ll help you compare realistic benefits, dosing, and how each fits beside core strengthening and posture work. LLLT may complement your plan when used intentionally, not as a stand-alone.
What does the evidence actually say?
A candid summary: evidence is encouraging but mixed, and results vary by device, protocol, and patient type. Some controlled studies report meaningful improvements in low back pain and function; others show modest or no differences versus sham. That’s normal with emerging, non-drug therapies especially when protocols aren’t standardized.
What matters for you is a smart trial: a time-bounded, well-structured attempt with clear checkpoints so you can tell whether this tool belongs in your toolkit. If you combine electromagnetic pulse therapy for back pain with the basics (gradual movement, ergonomic fixes, and good sleep), you give it a fair chance to help.
Who is a good candidate?
You might consider a PEMF trial if you have:
-
Mechanical low back pain (muscle strain, facet irritation, postural overload).
-
Subacute pain that lingers after a strain but isn’t worsening.
-
Chronic, nagging stiffness where you’re seeking a non-drug adjunct.
-
Sensitivity to medications, or you prefer non-pharmacologic first steps.
-
A plan for movement, like gentle core activation or walking PEMF pairs well with “active recovery.”
If you’ve had recent trauma, fever, unexplained weight loss, progressive weakness, or changes in bladder/bowel control, pause here and get medical evaluation first. A safe plan starts with ruling out red flags.
PEMF Therapy Benefits — Before you book extra sessions, skim this explainer to understand where PEMF helps, where it’s neutral, and when you should prioritize core work or targeted therapy instead. It frames expectations so you’ll judge progress by function—walking, lifting, sleep—rather than just time on a device.
Who should get medical clearance first or skip it?

For safety, electromagnetic pulse therapy for back pain generally isn’t used in people with:
-
Pacemakers, implanted defibrillators, or other electronic implants (fields can interfere).
-
Pregnancy (out of caution, as robust safety data are limited).
-
Uncontrolled seizures or certain active bleeding conditions.
-
Active malignancy in the treatment field, unless your treating physician says otherwise.
If you have orthopedic metal (e.g., screws or rods), many PEMF systems can be used safely, but you should still confirm device guidance and ask your clinician.
What does a sensible PEMF program look like?
You’ll see many protocols. A conservative, neurologist-approved approach is:
-
Set a trial window of 2–4 weeks.
-
Start low and slow: short sessions (e.g., 10–20 minutes), moderate settings.
-
Track three metrics every few days: average pain (0–10), morning stiffness (0–10), and “ease of movement” (0–10).
-
Pair with light activity: daily walking, gentle mobility, and two short core-stability exercises you can do without pain.
-
Advance gradually: if you’re symptom-stable or improving, lengthen sessions or add one extra session per week.
If your metrics are flat or worse after the trial, electromagnetic pulse therapy for back pain may not be your tool and that’s okay. The goal is clarity.
What will I feel during a session?
Most people feel very little: sometimes a faint tapping or warmth from the applicator, more often nothing at all. What matters is how you feel after: easier bending, a little less guarding, slightly more freedom getting in/out of the car. Look for small wins that accumulate.
Possible side effects are uncommon and usually mild temporary soreness, a “worked-out” feeling, or transient lightheadedness if you stand too quickly after relaxing. Stop if anything feels off and talk with your clinician.
How does PEMF compare with heat, TENS, or exercise?

They’re different tools:
-
Heat relaxes surface tissues and feels soothing; great before gentle mobility.
-
TENS (electrical stimulation) acts mainly on nerve pathways at the skin; some people love it, others don’t.
-
Exercise reshapes the long-term landscape strength, coordination, and resilience.
Electromagnetic pulse therapy for back pain tries to influence deeper cellular environments. The best results often happen when you stack tools wisely: brief PEMF, then easy mobility or core work, then a short walk. Synergy beats any single trick.
A 2-week, step-by-step home trial (print this)
Day 1–3 (Foundation)
-
Session: 10–15 minutes, moderate setting.
-
Movement: 2×/day five-minute mobility (pelvic tilts, cat-camel, gentle thoracic rotations).
-
Walk: 10 minutes at a relaxed pace.
-
Track: pain, stiffness, ease of movement.
Day 4–7 (Consistency)
-
Session: 15–20 minutes.
-
Movement: keep mobility; add 2×10 of easy core (dead bug or bird-dog, whichever is pain-free).
-
Walk: 12–15 minutes.
-
Checkpoint: if scores are trending down by even 1 point, you’re on track.
Day 8–10 (Build)
-
Session: 20 minutes.
-
Movement: keep core; add hip hinge drills with a dowel to relearn bending mechanics.
-
Walk: 15–20 minutes.
Day 11–14 (Decide)
-
Session: maintain.
-
Movement: begin light “carry” work (a small grocery bag in one hand for 30–60 seconds, switch sides).
-
Walk: 20 minutes.
-
Decision: if pain and stiffness are down ≥2 points and you’re moving easier, PEMF earned a spot in your toolkit. If not, close the trial and pivot no guilt, just data.
This structure helps you test electromagnetic pulse therapy for back pain without drifting into endless “maybe.”
How to choose a device or clinic without the hype
-
Adjustability matters: ability to tweak intensity and session length.
-
Clarity beats claims: look for straightforward explanations, not miracle language.
-
Comfort and consistency: a device you’ll actually use beats a perfect one that gathers dust.
-
Professional guidance: if you’re unsure, work with a clinician who understands spine mechanics and can integrate PEMF into a complete plan.
Your whole-back plan: the five pillars
-
Motion is medicine: short, frequent movement wins over long, heroic sessions.
-
Core coordination, not crunches: bird-dog, dead bug, side planks pain-free versions only.
-
Hip mobility first: hips that move well protect your back.
-
Smart ergonomics: chair height, screen position, and micro-breaks every 30–45 minutes.
-
Sleep and stress care: your nervous system heals when you do.
Layer electromagnetic pulse therapy for back pain onto these pillars and you’ll give yourself a real chance at momentum.
Motivation check: you’re not behind
Healing is not linear, and it’s not a race. If you’re reading this, you’re already doing the bravest thing staying engaged. Whether PEMF becomes your favorite tool or just something you tried on the way to better answers, you’re moving forward. I’m proud of you for that.
Summary
Electromagnetic pulse therapy for back pain is a noninvasive option that may support tissue recovery, reduce guarding, and ease pain for some people especially when paired with movement, ergonomics, and healthy sleep. The science is promising but not definitive; results depend on the person, device, and protocol. The smartest approach is a structured 2–4 week trial with clear metrics. If you improve, keep it. If not, pivot confidently. You’re not stuck; you’re learning what works for your body.
Frequently Asked Questions
1) Does electromagnetic pulse therapy for back pain really work?
It can for some people, especially with mechanical low back pain. Benefits are typically modest but meaningful less morning stiffness, easier transitions, and better tolerance for gentle exercise. A structured trial is the best way to know.
2) Is electromagnetic pulse therapy for back pain safe?
Generally yes for many adults when used as directed, but avoid it if you have implanted electronic devices, are pregnant, or have specific medical conditions without clinician approval. Stop if anything feels off.
3) How soon would I feel changes?
Some notice “easier movement” after a few sessions; others need 1–2 weeks. Track your metrics so you can tell whether change is real.
4) Can I use PEMF with other therapies?
Yes. It pairs well with heat, gentle mobility, and graded walking. Many people do a brief PEMF session, then movement exercises while tissues feel calmer.
5) Is electromagnetic pulse therapy for back pain the same as TENS?
No. TENS uses surface electrical stimulation; PEMF uses magnetic fields to induce tiny currents deeper in tissues. Both can be part of a non-drug pain plan.
6) How long should each session be?
Many protocols use 10–20 minutes to start. Longer isn’t always better consistency and pairing with movement matter more.
7) If my pain is from a disc bulge or sciatica, can I try it?
Some people with disc-related pain report relief, but responses vary widely. Start only after a clinician confirms it’s appropriate for your specific pattern and there are no red flags.
8) Will electromagnetic pulse therapy for back pain fix my posture?
It won’t directly change posture, but by reducing guarding and stiffness, it can make posture work and mobility drills more comfortable so you can actually practice them.
9) Can I overdo it?
Yes. If you ramp settings or duration too quickly, you may feel sore or fatigued. Start low, go slow, and let your symptom log guide you.
10) What if I don’t improve after two weeks?
You learned something valuable. Close the trial, and shift focus to other evidence-based options like targeted exercise progressions, ergonomics, and nervous-system-calming strategies.
👨⚕️ Alireza Chizari, MSc, DC, DACNB
🧠 Clinical Focus
🔬 Assessment & Treatment Approach
Objective testing may include:
Treatment programs may involve:
📍 Clinic Information
✅ Medical Review
⚠️ Disclaimer
Comments
FAQ
What is Functional Neurology?
Functional Neurology is a healthcare specialty that focuses on assessing and rehabilitating the nervous system’s function. It emphasizes neuroplasticity—the brain’s ability to adapt and reorganize—using non-invasive, evidence-based interventions to improve neurological performance.
How does Functional Neurology differ from traditional neurology?
Traditional neurology often concentrates on diagnosing and treating neurological diseases through medications or surgery. In contrast, Functional Neurology aims to optimize the nervous system’s function by identifying and addressing dysfunctions through personalized, non-pharmaceutical interventions.
Is Functional Neurology a replacement for traditional medical care?
No. Functional Neurology is intended to complement, not replace, traditional medical care. Practitioners often collaborate with medical professionals to provide comprehensive care.
What conditions can Functional Neurology help manage?
Functional Neurology has been applied to various conditions, including:
• Concussions and Post-Concussion Syndrome
• Traumatic Brain Injuries (TBI)
• Vestibular Disorders
• Migraines and Headaches
• Neurodevelopmental Disorders (e.g., ADHD, Autism)
• Movement Disorders
• Dysautonomia
• Peripheral Neuropathy
• Functional Neurological Disorder (FND)
Can Functional Neurology assist with neurodegenerative diseases?
While Functional Neurology does not cure neurodegenerative diseases, it can help manage symptoms and improve quality of life by optimizing the function of existing neural pathways.
What diagnostic methods are used in Functional Neurology?
Functional Neurologists employ various assessments, including:
• Videonystagmography (VNG)
• Computerized Posturography
• Oculomotor Testing
• Vestibular Function Tests
• Neurocognitive Evaluations
How is a patient’s progress monitored?
Progress is tracked through repeated assessments, patient-reported outcomes, and objective measures such as balance tests, eye movement tracking, and cognitive performance evaluations.
What therapies are commonly used in Functional Neurology?
Interventions may include:
- Vestibular Rehabilitation
- Oculomotor Exercises
- Sensorimotor Integration
- Cognitive Training
- Balance and Coordination Exercises
- Nutritional Counseling
- Lifestyle Modifications
Are these therapies personalized?
Absolutely. Treatment plans are tailored to the individual’s specific neurological findings, symptoms, and functional goals.
Who can benefit from Functional Neurology?
Individuals with unresolved neurological symptoms, those seeking non-pharmaceutical interventions, or patients aiming to optimize brain function can benefit from Functional Neurology.
Is Functional Neurology suitable for children?
Yes. Children with developmental delays, learning difficulties, or neurodevelopmental disorders may benefit from Functional Neurology approaches.
How does Functional Neurology complement other medical treatments?
It can serve as an adjunct to traditional medical care, enhancing outcomes by addressing functional aspects of the nervous system that may not be targeted by conventional treatments.
How is technology integrated into Functional Neurology?
Technological tools such as virtual reality, neurofeedback, and advanced diagnostic equipment are increasingly used to assess and enhance neurological function.
What is the role of research in Functional Neurology?
Ongoing research continues to refine assessment techniques, therapeutic interventions, and our understanding of neuroplasticity, contributing to the evolution of Functional Neurology practices.

Dr. Alireza Chizari
Latest articles

