If you live in or near Hidden Hills and feel like the room spins while your head pounds, you are not alone. Many people quietly push through episodes of migraine and vertigo, wondering if they are overreacting or simply stressed, while their world becomes smaller and more unpredictable.
I am Dr. Alireza Chizari, and in this article I will walk you through how we think about migraine with vertigo treatment in Hidden Hills and the surrounding area. My goal is to help you understand what might be happening in your brain and inner ear, what a careful evaluation looks like, and which non invasive therapies we can use to help you feel more stable, confident, and in control again.
Non Invasive Migraine with Vertigo Treatment in Hidden Hills
You are the hero of this story. You are the one who has kept working, caring for your family, and showing up despite dizzy spells and pounding headaches. My role, and the role of our team at California Brain & Spine Center in Calabasas, is to be your guide and partner, using advanced neurological and vestibular tools to support your healing.
If you are looking for migraine with vertigo treatment in Hidden Hills that is scientific, personalized, and non invasive, this page will show you what your next steps can be and how we can help.
Migraine with vertigo treatment in Hidden Hills – why your symptoms matter
When migraine and vertigo come together, it can feel frightening and strange. You might feel:
-
A spinning or rocking sensation, even when you are still
-
Pressure or pain on one side of the head
-
Sensitivity to light, sound, or busy visual environments
-
Nausea, imbalance, or a sense that your body is “off”
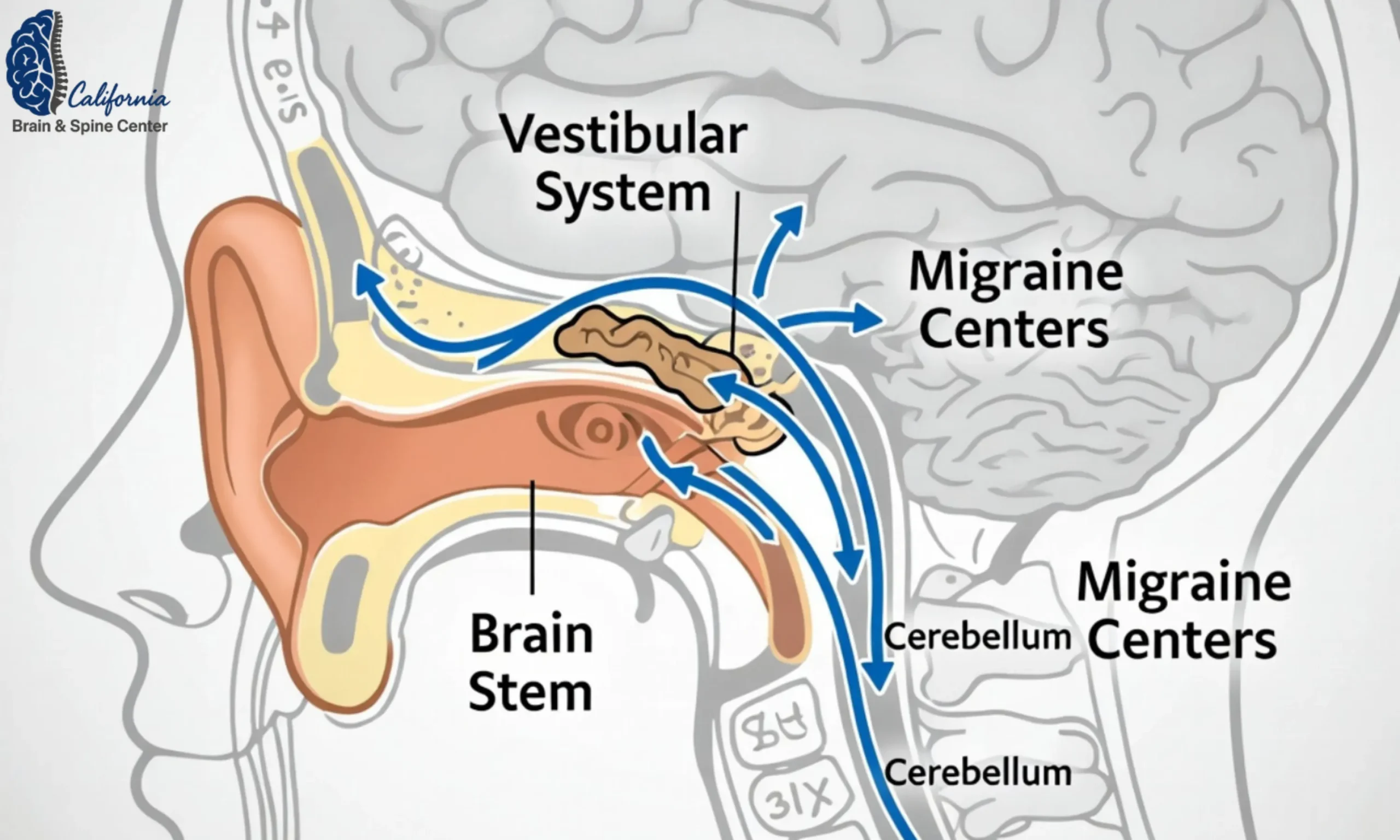
In many cases, this pattern fits what is called vestibular migraine, a type of migraine where dizziness, vertigo, and balance problems are prominent symptoms. Research suggests that vestibular migraine is one of the most common causes of recurrent spontaneous vertigo and is linked with disruption of how the brain and inner ear process motion and sensory input.
From my perspective as a clinician trained in both engineering and clinical neuroscience, your symptoms are signals of how your nervous system is processing overload, not a sign that you are “weak” or “dramatic.” When I work with patients from Hidden Hills, I see people who have been forced to reorganize their lives around unpredictable attacks:
-
Avoiding driving on the freeway
-
Cancelling social plans because of light and sound sensitivity
-
Struggling to work on screens without feeling sick
Migraine with vertigo treatment in Hidden Hills must start by respecting how disruptive this is to your life and by taking your story seriously.

How to recognize migraine with vertigo symptoms in everyday life
Many patients come to me after months or years of feeling dismissed. They have been told they have “sinus issues,” “stress,” or “ear crystals,” while their symptoms do not fully match those explanations. Recognizing the pattern of migraine with vertigo can be the first empowering step.
Some common features, based on current knowledge about vestibular migraine, include: Hopkins Medicine+1
-
Episodes of vertigo or dizziness that last minutes to hours, sometimes longer
-
Imbalance or a feeling of walking on a boat
-
Nausea, sometimes vomiting
-
Sensitivity to light, sound, or complex visual patterns
-
Headache that may be throbbing, often one sided, but sometimes mild or absent
-
A history of migraine, motion sickness, or strong reactions to visual or sensory triggers
You may notice patterns, such as:
-
Symptoms triggered by certain foods, hormonal shifts, sleep disruption, or stress
-
Worsening with busy visual input, like grocery store aisles or scrolling screens
-
Feeling “hungover” or drained for a day or more after an episode
If you recognize yourself in this description and you live in Hidden Hills or nearby, it is worth considering a focused evaluation rather than assuming this is something you “just have to live with.”
Healing starts the moment you stop blaming yourself for your symptoms and start seeing them as information your nervous system is giving you.
How California Brain & Spine Center evaluates migraine with vertigo for Hidden Hills patients
At California Brain & Spine Center in Calabasas, patients seeking migraine with vertigo treatment in Hidden Hills are evaluated with a structured, engineering minded approach. Instead of looking at your symptoms in isolation, the team views your brain, inner ear, and autonomic nervous system as an integrated network.
Step 1 – Detailed story and trigger mapping
Patients are guided through a thorough history that explores:
-
Onset and evolution of headaches, vertigo, and dizziness
-
Specific triggers such as visual motion, hormonal shifts, stress, or certain foods
-
Past head or neck injuries, even “minor” concussions or whiplash
-
Sleep patterns, fatigue, brain fog, and cognitive changes
-
Coexisting issues like neck pain, tinnitus, palpitations, or digestive problems
This engineering style history looks for patterns, not just isolated complaints. A person from Hidden Hills who has “migraine with vertigo” might actually have contributions from vestibular migraine, old concussion, cervical spine dysfunction, or autonomic dysregulation. The goal is to map the system, not slap on a label.
Step 2 – Advanced vestibular, neurological, and autonomic testing
Depending on the case, the clinical team may use:
-
Bedside vestibular tests to assess eye movements, balance, and gaze stability
-
Positional testing to rule in or rule out conditions like BPPV or inner ear inflammation
-
Cognitive screening when brain fog or memory issues are present
-
Autonomic nervous system assessment for patients with lightheadedness, heart rate changes, or suspected dysautonomia
-
Posture and cervical spine evaluation, especially in those with neck pain or whiplash history
For complex cases, this may be complemented by neurologist reports, imaging ordered by your medical doctor, or other specialist input. The goal is not to repeat tests you already had, but to connect the dots in a neurological and vestibular framework.
The right diagnosis is rarely a single word. It is a clear picture of how all the pieces of your nervous system fit together.

Non invasive migraine with vertigo treatment options in Hidden Hills
Once a clear picture has been built, migraine with vertigo treatment in Hidden Hills focuses on gentle, evidence informed, non invasive approaches that support neuroplasticity, not just symptom suppression.
At California Brain & Spine Center, patients may receive a personalized combination of:
Vestibular rehabilitation and NeuroSensory Integration
Vestibular rehabilitation uses carefully designed exercises to help the brain recalibrate how it processes motion, head position, and visual input. For patients with migraine and vertigo, this is done thoughtfully to avoid provoking flare ups while still nudging the nervous system toward adaptation. Studies show that targeted vestibular rehab can reduce dizziness and imbalance in various vestibular disorders.
NeuroSensory Integration (NSI) builds on this by working with:
-
Eye movement and visual tracking
-
Head and neck coordination
-
Balance, gait, and spatial orientation
-
Sensory integration between visual, vestibular, and proprioceptive inputs
By reshaping how these systems work together, NSI helps many patients feel less overwhelmed by busy environments and motion stimuli.
Targeted neuromodulation – LLLT, PEMF, HBOT, GammaCore, NeuroRevive
In selected cases, non invasive neurology therapies are added to support brain healing and modulation of pain pathways. These may include:
-
Low-Level Laser Therapy (LLLT) to modulate local blood flow and cellular activity
-
Pulsed Electromagnetic Field (PEMF) therapy to influence cellular signaling and neuroplasticity
-
Hyperbaric Oxygen Therapy (HBOT) to increase oxygen delivery to injured or sensitive brain regions
-
GammaCore vagus nerve stimulation to help regulate pain and autonomic tone
-
The NeuroRevive Program, which combines specific neuromodulation tools with tailored exercises and cognitive support
These modalities are not used in a “one size fits all” way. They are integrated into a plan based on each patient’s history, sensitivity level, and goals. For example, someone from Hidden Hills with frequent vestibular migraine flares may start with gentler vestibular work and short neuromodulation sessions, progressing only as their system tolerates.
Technology is powerful, but it is most healing when it is guided by a deep understanding of the person in front of us, not just their diagnosis.

Building a long term plan so you can trust your body again
Now I want to return to first person, because this is where your story and my role as your guide come together.
When I work with patients searching for migraine with vertigo treatment in Hidden Hills, the true goal is not simply “fewer episodes.” The real goal is for you to rebuild trust in your body, so that:
-
You can drive with more confidence
-
You can enter a grocery store or busy environment without fear
-
You can plan your life without constantly worrying about the next flare
For many people, this happens in stages:
-
Stabilization – Reducing the intensity and frequency of acute attacks, addressing red flags, and making sure nothing dangerous is being missed.
-
Recalibration – Using vestibular rehabilitation, NSI, and neuromodulation to help your brain process motion and sensory input more effectively.
-
Resilience – Strengthening your system so that triggers like stress, travel, screen time, or hormonal shifts are less likely to push you into a full flare.
Between visits, I often encourage patients to focus on a few key habits:
-
Protecting consistent sleep and wake times
-
Gentle, regular movement rather than long periods of inactivity
-
Hydration and regular meals to support autonomic stability
-
Noticing early warning signs and responding sooner, rather than pushing through until an episode becomes severe
These are not meant to shift responsibility onto you. Instead, they are tools that allow you to play an active role in your own recovery while we guide the clinical side.

A real story from a Hidden Hills patient
Some time ago, a patient in her early 40s from Hidden Hills came to see me after two years of living with disabling migraine and vertigo. She had stopped driving on the highway, avoided bright stores, and felt like she was failing her family because she often needed to lie down in a dark room.
She had been told she had “anxiety” and “sinus headaches,” but her symptoms included spinning episodes, imbalance, nausea, and sensitivity to light and sound. After a detailed neurological and vestibular evaluation, it became clear that she had a pattern consistent with vestibular migraine, with contributions from an old whiplash injury and mild autonomic dysregulation.
We built a plan that included gentle vestibular rehabilitation, NeuroSensory Integration, neck and posture work, and carefully titrated neuromodulation with elements of the NeuroRevive Program. As her system adapted, we gradually added more challenging visual and balance tasks.
Over several months, her migraine with vertigo episodes shifted from weekly to rare. She started driving longer distances again and was able to attend her child’s school events without fear of collapsing or needing to leave suddenly. She told me, “I finally feel like my world is opening back up again.”
Her story does not mean every patient will follow the same timeline or outcome, but it is a real example of what can happen when migraine with vertigo treatment in Hidden Hills is approached with precision, respect, and a neuroplasticity focused plan.
Your most common questions about migraine with vertigo treatment in Hidden Hills
Q1: How do I know if my dizziness and headaches are really migraine with vertigo and not just an inner ear problem?
A: It can be difficult to tell on your own. Vestibular migraine often includes episodes of vertigo, imbalance, and sensory sensitivity that may or may not occur with strong head pain. Inner ear problems like BPPV or labyrinthitis tend to have specific patterns related to head position or infection history. A detailed history plus vestibular and neurological testing is usually needed to distinguish these conditions. If your symptoms are recurrent, triggered by stress, hormones, visual motion, or certain foods, and you have a migraine history, it is worth being evaluated for vestibular migraine as part of your workup.
Q2: Is migraine with vertigo dangerous or life threatening?
A: Migraine with vertigo is usually not life threatening by itself, but its symptoms can be very disabling. However, certain “red flag” symptoms such as sudden severe headache, weakness on one side, difficulty speaking, chest pain, or new neurological changes require immediate emergency evaluation, because they can overlap with more serious conditions. Part of a responsible evaluation is making sure these dangerous possibilities are ruled out or appropriately addressed before focusing on vestibular migraine treatment.
Q3: What does a typical treatment plan look like at your clinic for someone from Hidden Hills?
A: After a careful evaluation, a plan may combine vestibular rehabilitation, NeuroSensory Integration, neck and posture care, and non invasive neuromodulation tools like LLLT, PEMF, HBOT, or GammaCore when appropriate. The pace and intensity are adjusted based on your sensitivity and response. In the beginning, visits may be more frequent as we guide your brain and inner ear toward better integration. Over time, sessions are spaced out as you gain stability and confidence.
Q4: Will I have to do these exercises forever?
A: Most patients do not need intensive exercises forever. There is usually a more active phase while your nervous system is recalibrating, followed by a maintenance phase where you use a few simple strategies during times of higher stress, travel, or hormonal change. Think of it like physical therapy for your brain and balance system. Once you rebuild capacity, you often only need brief refreshers during more challenging periods.
Q5: Can I continue my usual migraine medication while doing this kind of treatment?
A: In many cases, yes. Medication decisions are always coordinated with your prescribing physician or neurologist. Non invasive therapies such as vestibular rehab, NSI, and neuromodulation are typically compatible with standard migraine medications. Sometimes, as function improves, patients and their physicians choose to adjust doses, but that is always done carefully and under medical supervision.
Conclusion – your next step toward calmer, steadier days
As you can see, migraine with vertigo treatment in Hidden Hills is about much more than chasing individual symptoms. It is about understanding how your brain, inner ear, neck, and autonomic nervous system are working together and then guiding that system toward a more stable pattern.
In this article, I have shared how we think about vestibular migraine and related conditions, how a careful evaluation is performed, and how non invasive tools like vestibular rehabilitation, NeuroSensory Integration, LLLT, PEMF, HBOT, GammaCore, and the NeuroRevive Program can support your recovery. Most importantly, I hope you now see that your symptoms are real, understandable, and worthy of expert attention.
If all you remember from this page is this, it is enough: you are not “too sensitive” or imagining things, and there are structured, scientific ways to help your brain and body feel safer and more balanced again.
As a clinician who has moved from engineering into neuroscience and chiropractic care, my commitment is to combine precise thinking with compassionate listening. You are the hero of this journey. My role is to walk alongside you with the best tools we have.
If you feel ready to take the next step, I invite you to contact our clinic in Calabasas to explore whether our approach is right for you.
If you live in Hidden Hills or anywhere in the surrounding areas and you recognize yourself in this description of migraine with vertigo, you do not have to keep guessing on your own. You can reach out to California Brain & Spine Center to schedule a personalized neurological and vestibular evaluation, discuss your goals, and design a plan that supports the best version of your life and function, not just the suppression of isolated symptoms.
👨⚕️ Alireza Chizari, MSc, DC, DACNB
🧠 Clinical Focus
🔬 Assessment & Treatment Approach
Objective testing may include:
Treatment programs may involve:
📍 Clinic Information
✅ Medical Review
⚠️ Disclaimer
Comments
FAQ
What is Functional Neurology?
Functional Neurology is a healthcare specialty that focuses on assessing and rehabilitating the nervous system’s function. It emphasizes neuroplasticity—the brain’s ability to adapt and reorganize—using non-invasive, evidence-based interventions to improve neurological performance.
How does Functional Neurology differ from traditional neurology?
Traditional neurology often concentrates on diagnosing and treating neurological diseases through medications or surgery. In contrast, Functional Neurology aims to optimize the nervous system’s function by identifying and addressing dysfunctions through personalized, non-pharmaceutical interventions.
Is Functional Neurology a replacement for traditional medical care?
No. Functional Neurology is intended to complement, not replace, traditional medical care. Practitioners often collaborate with medical professionals to provide comprehensive care.
What conditions can Functional Neurology help manage?
Functional Neurology has been applied to various conditions, including:
• Concussions and Post-Concussion Syndrome
• Traumatic Brain Injuries (TBI)
• Vestibular Disorders
• Migraines and Headaches
• Neurodevelopmental Disorders (e.g., ADHD, Autism)
• Movement Disorders
• Dysautonomia
• Peripheral Neuropathy
• Functional Neurological Disorder (FND)
Can Functional Neurology assist with neurodegenerative diseases?
While Functional Neurology does not cure neurodegenerative diseases, it can help manage symptoms and improve quality of life by optimizing the function of existing neural pathways.
What diagnostic methods are used in Functional Neurology?
Functional Neurologists employ various assessments, including:
• Videonystagmography (VNG)
• Computerized Posturography
• Oculomotor Testing
• Vestibular Function Tests
• Neurocognitive Evaluations
How is a patient’s progress monitored?
Progress is tracked through repeated assessments, patient-reported outcomes, and objective measures such as balance tests, eye movement tracking, and cognitive performance evaluations.
What therapies are commonly used in Functional Neurology?
Interventions may include:
- Vestibular Rehabilitation
- Oculomotor Exercises
- Sensorimotor Integration
- Cognitive Training
- Balance and Coordination Exercises
- Nutritional Counseling
- Lifestyle Modifications
Are these therapies personalized?
Absolutely. Treatment plans are tailored to the individual’s specific neurological findings, symptoms, and functional goals.
Who can benefit from Functional Neurology?
Individuals with unresolved neurological symptoms, those seeking non-pharmaceutical interventions, or patients aiming to optimize brain function can benefit from Functional Neurology.
Is Functional Neurology suitable for children?
Yes. Children with developmental delays, learning difficulties, or neurodevelopmental disorders may benefit from Functional Neurology approaches.
How does Functional Neurology complement other medical treatments?
It can serve as an adjunct to traditional medical care, enhancing outcomes by addressing functional aspects of the nervous system that may not be targeted by conventional treatments.
How is technology integrated into Functional Neurology?
Technological tools such as virtual reality, neurofeedback, and advanced diagnostic equipment are increasingly used to assess and enhance neurological function.
What is the role of research in Functional Neurology?
Ongoing research continues to refine assessment techniques, therapeutic interventions, and our understanding of neuroplasticity, contributing to the evolution of Functional Neurology practices.

Dr. Alireza Chizari
Latest articles

