Early Warning Signs of Central Vestibular Disorders
At our California Brain & Spine Center in Calabasas, I meet a certain kind of dizzy patient over and over: someone who has been told “it’s just vertigo” or “probably the ear,” but the story doesn’t fully match a simple inner-ear problem. Maybe their speech felt thick for a few minutes, maybe their walking was off, maybe their vision doubled briefly. Those are the moments when my antenna goes up, because they can be early warning signals the kind of symptoms we group under the phrase Early Warning Signs of Central Vestibular Disorders. These are not the patients we want to send home with only positional exercises and hope for the best. These are the patients we screen more carefully.
This article is for that group: people in California who have dizziness that doesn’t behave like typical BPPV, or who have other neurological symptoms at the same time. I’ll explain what counts as Early Warning Signs of Central Vestibular Disorders, how to tell dizziness that requires MRI (not peripheral), and when dizziness suggests brainstem or cerebellar cause instead of a simple vestibular ear problem. If you recognize yourself in these patterns, it’s worth being evaluated in a clinic that actually works with central vestibular symptoms (diplopia, dysarthria, ataxia) every week.
Catching central vestibular problems early gives your brain its best chance to adapt and recover. In our care for vestibular dysfunction, we use advanced eye movement and balance testing to identify which areas of the brain are not processing motion correctly, then design highly specific rehab to stabilize your world again. This is especially important for patients who already notice early warning signs but have not received a clear explanation for them.
VNG Testing That Reveals Hidden Central Vestibular Dysfunction
This video explains why many patients remain dizzy even when MRI or CT scans appear normal. VNG testing measures how the brain, eyes, and vestibular system work together, helping uncover central vestibular problems that routine imaging often misses. For patients and attorneys, VNG provides objective, measurable data that guides accurate treatment and documents neurological impairment with clinical clarity.
Central vs Peripheral: Why We Care So Much
Most vertigo is peripheral. It comes from the inner ear, it’s positional, it’s intense but short, and it often responds to simple maneuvers or vestibular rehab. But Early Warning Signs of Central Vestibular Disorders point to the brainstem, cerebellum, or central pathways that process balance. Those structures are too important to ignore.
Here’s the key clinical idea: peripheral vertigo is often dramatic but safe; central vertigo can be subtle but serious. That’s why we teach patients to notice red flags for central vertigo and not to dismiss them just because they only lasted a few minutes.
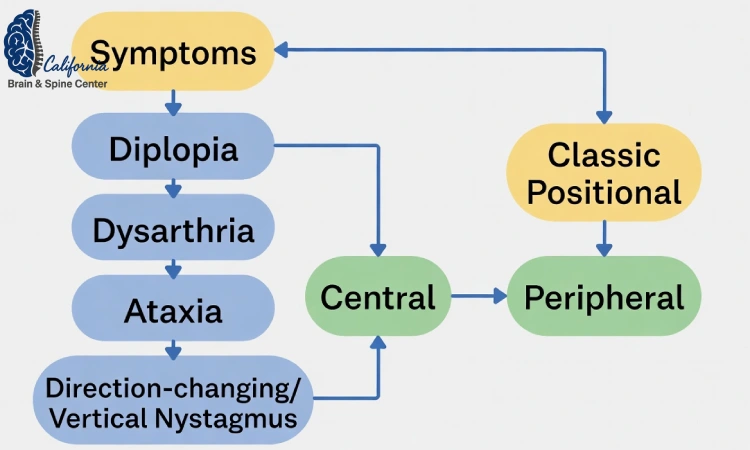
The Core Early Warning Signs of Central Vestibular Disorders
Let’s go through the features we do not brush off. If a patient reports one or more of these, we start thinking about dizziness that requires MRI (not peripheral):
-
Transient or persistent double vision (diplopia)
-
Slurred or effortful speech (dysarthria)
-
Trouble coordinating movements or walking like they’re “pulled” to one side (ataxia)
-
Vertigo that is not clearly triggered by head position
-
Vertigo accompanied by new weakness or numbness
-
Direction-changing or vertical eye movements
-
Sudden onset in a person with vascular risk factors
Each of those can show up early, before a larger neurological event. That’s why we call them Early Warning Signs of Central Vestibular Disorders they tell us the balance problem may be coming from the brain, not the ear.
Central vestibular disorders often start with small changes that are easy to dismiss, like subtle unsteadiness, difficulty tolerating busy visual environments, or feeling “off” when turning your head. Over time these early warning signs can point to more serious conditions that deserve careful evaluation. If you are unsure when dizziness crosses the line from annoying to potentially concerning, our article on when dizziness needs neuroimaging and specialist referral outlines red flags that should not be ignored and explains how we decide which tests are truly necessary.
Dizziness That Requires MRI (Not Peripheral)
Patients often ask, “How do I know when it’s time for a scan?” We don’t scan every dizzy person that would be wasteful and anxiety-provoking. But there is a clear group of cases of dizziness that requires MRI (not peripheral):
-
The dizziness is accompanied by central vestibular symptoms (diplopia, dysarthria, ataxia).
-
The nystagmus is vertical or changes direction with gaze.
-
The dizziness does not fatigue and is not reproducible with classic BPPV tests.
-
There is a sudden onset of imbalance without ear symptoms.
-
There is a known or suspected brainstem or cerebellar lesion.
-
Symptoms do not improve with appropriate vestibular treatment.
In other words, when dizziness suggests brainstem or cerebellar cause, or when we see red flags for central vertigo, we do not keep treating it like a peripheral problem. We escalate.
What “Brainstem or Cerebellar Cause” Looks Like
A lot of people hear “brainstem” or “cerebellum” and imagine a huge dramatic stroke. Sometimes it is dramatic, but sometimes it’s much earlier than that. Here are common ways when dizziness suggests brainstem or cerebellar cause:

-
You feel like you’re tilting or drifting even when sitting still.
-
One side of your face or tongue felt odd during the episode.
-
You couldn’t walk in a straight line not just “a little off,” but really unsteady.
-
Your eyes jumped in an unusual way when you looked to the side.
-
You had a short episode of slurred speech along with vertigo.
Put together, those are Early Warning Signs of Central Vestibular Disorders. They tell us the balance center in the brain or the pathways connecting it are irritated, inflamed, or lacking blood flow and those are not places we ignore.
How We Evaluate These Patients in Calabasas
Because we see a lot of post-concussion and complex dizziness patients in Southern California, we’ve built a workflow that doesn’t miss central signs.
-
We listen to the exact symptom sequence central problems often have “and then I couldn’t walk right” or “my eyes crossed for a second.”
-
We do bedside ocular and vestibular tests to look for central vestibular symptoms (diplopia, dysarthria, ataxia-related gaze problems).
-
We rule out simple BPPV with positional tests so we don’t confuse a peripheral issue with a central one.
-
If the story or exam doesn’t match a peripheral pattern, we talk about imaging or neurology co-management.
That’s the advantage of being seen in a clinic that actually treats dizziness every day: we can tell you when your dizziness is in the safe group, and when it’s in the group of dizziness that requires MRI (not peripheral).
Why Central Vestibular Signs Get Missed
Central problems get missed because they can be subtle and intermittent. A patient might have dysarthria for 2 minutes and then sound normal. They might have ataxia only when they’re tired. They might have double vision only when looking far right. But intermittent doesn’t mean unimportant. Intermittent can be early.
That’s why we tell patients to write down episodes that feel like red flags for central vertigo timing, triggers, duration, other neurological symptoms. A pattern of small central signs is still a pattern.
Linking to Dysautonomia and Post-Concussion Cases

In our population, we see another twist: patients who already have dysautonomia or who are recovering from concussion. Their nervous systems are already sensitive. When they develop imbalance, everyone assumes it’s “just the concussion.” But sometimes these patients show Early Warning Signs of Central Vestibular Disorders on top of their existing problem. If they suddenly develop central vestibular symptoms (diplopia, dysarthria, ataxia), we do not blame it on anxiety or whiplash we evaluate it properly.
So even if you’ve already been diagnosed with vestibular dysfunction or post-concussion syndrome, pay attention to when dizziness suggests brainstem or cerebellar cause. New central signs deserve new attention.
When to Seek In-Person Care
You should be evaluated in person for example at our clinic in Calabasas if:
-
Your dizziness is not clearly positional.
-
You have had speech, vision, or walking changes at the same time.
-
You have risk factors for stroke and the dizziness came on suddenly.
-
You failed to improve with typical vestibular treatments.
-
You are unsure whether this is peripheral or central.
Those are the situations where Early Warning Signs of Central Vestibular Disorders actually help us pick the right pathway: rehab vs imaging vs neurology.
If you live in Calabasas, elsewhere in Los Angeles County, or you travel to us from Southern California, and you’ve had dizziness that does not behave like a simple ear problem especially if you noticed central vestibular symptoms (diplopia, dysarthria, ataxia) or other red flags for central vertigo our team can evaluate you. We will tell you whether this is a case that fits non-invasive vestibular rehabilitation and post-concussion care, or whether it looks more like dizziness that requires MRI (not peripheral) and needs coordination with a neurologist.
You can review our services and learn about our approach at https://californiabrainspine.com/ our experts will help you move toward an accurate diagnosis and an actionable plan.
Summary
Early Warning Signs of Central Vestibular Disorders are the brain’s way of telling you “this dizziness is not just inner ear.” When dizziness suggests brainstem or cerebellar cause, or when you see central vestibular symptoms (diplopia, dysarthria, ataxia), or when you experience dizziness that requires MRI (not peripheral), it’s time to step out of the generic vertigo pathway and get a neurologically informed evaluation. Clinics like ours in Calabasas are built to make that distinction and to connect you to the right non-invasive neurology, vestibular, or concussion program.
FAQs
1. How do I know if my dizziness is central or peripheral?
If you have vision changes, speech difficulty, or trouble walking at the same time as dizziness, those are Early Warning Signs of Central Vestibular Disorders. Positional, short, predictable spinning attacks are more likely peripheral.
2. Does every central-looking dizziness mean stroke?
No, but central vestibular symptoms (diplopia, dysarthria, ataxia) tell us to rule out brainstem or cerebellar causes. That’s why some cases become dizziness that requires MRI (not peripheral).
3. Can BPPV cause slurred speech or double vision?
Typical BPPV does not. If you have those, you’re in the territory of red flags for central vertigo and should be evaluated in person.
4. What if my symptoms come and go?
Intermittent symptoms can still be Early Warning Signs of Central Vestibular Disorders, especially in patients with vascular risk factors or migraine variants. Track them and bring them to your evaluation.
5. Can your clinic help if imaging is normal?
Yes. Many patients have normal scans but still have central processing or vestibulo-ocular issues after concussion or mild brain injury. We can address those through non-invasive neurology and vestibular rehabilitation at https://californiabrainspine.com/.
👨⚕️ Alireza Chizari, MSc, DC, DACNB
🧠 Clinical Focus
🔬 Assessment & Treatment Approach
Objective testing may include:
Treatment programs may involve:
📍 Clinic Information
✅ Medical Review
⚠️ Disclaimer
Comments
FAQ
What is Functional Neurology?
Functional Neurology is a healthcare specialty that focuses on assessing and rehabilitating the nervous system’s function. It emphasizes neuroplasticity—the brain’s ability to adapt and reorganize—using non-invasive, evidence-based interventions to improve neurological performance.
How does Functional Neurology differ from traditional neurology?
Traditional neurology often concentrates on diagnosing and treating neurological diseases through medications or surgery. In contrast, Functional Neurology aims to optimize the nervous system’s function by identifying and addressing dysfunctions through personalized, non-pharmaceutical interventions.
Is Functional Neurology a replacement for traditional medical care?
No. Functional Neurology is intended to complement, not replace, traditional medical care. Practitioners often collaborate with medical professionals to provide comprehensive care.
What conditions can Functional Neurology help manage?
Functional Neurology has been applied to various conditions, including:
• Concussions and Post-Concussion Syndrome
• Traumatic Brain Injuries (TBI)
• Vestibular Disorders
• Migraines and Headaches
• Neurodevelopmental Disorders (e.g., ADHD, Autism)
• Movement Disorders
• Dysautonomia
• Peripheral Neuropathy
• Functional Neurological Disorder (FND)
Can Functional Neurology assist with neurodegenerative diseases?
While Functional Neurology does not cure neurodegenerative diseases, it can help manage symptoms and improve quality of life by optimizing the function of existing neural pathways.
What diagnostic methods are used in Functional Neurology?
Functional Neurologists employ various assessments, including:
• Videonystagmography (VNG)
• Computerized Posturography
• Oculomotor Testing
• Vestibular Function Tests
• Neurocognitive Evaluations
How is a patient’s progress monitored?
Progress is tracked through repeated assessments, patient-reported outcomes, and objective measures such as balance tests, eye movement tracking, and cognitive performance evaluations.
What therapies are commonly used in Functional Neurology?
Interventions may include:
- Vestibular Rehabilitation
- Oculomotor Exercises
- Sensorimotor Integration
- Cognitive Training
- Balance and Coordination Exercises
- Nutritional Counseling
- Lifestyle Modifications
Are these therapies personalized?
Absolutely. Treatment plans are tailored to the individual’s specific neurological findings, symptoms, and functional goals.
Who can benefit from Functional Neurology?
Individuals with unresolved neurological symptoms, those seeking non-pharmaceutical interventions, or patients aiming to optimize brain function can benefit from Functional Neurology.
Is Functional Neurology suitable for children?
Yes. Children with developmental delays, learning difficulties, or neurodevelopmental disorders may benefit from Functional Neurology approaches.
How does Functional Neurology complement other medical treatments?
It can serve as an adjunct to traditional medical care, enhancing outcomes by addressing functional aspects of the nervous system that may not be targeted by conventional treatments.
How is technology integrated into Functional Neurology?
Technological tools such as virtual reality, neurofeedback, and advanced diagnostic equipment are increasingly used to assess and enhance neurological function.
What is the role of research in Functional Neurology?
Ongoing research continues to refine assessment techniques, therapeutic interventions, and our understanding of neuroplasticity, contributing to the evolution of Functional Neurology practices.

Dr. Alireza Chizari
Latest articles

