If you live in or near Thousand Oaks and you wake up already bracing for another headache, you are not imagining things and you are not alone. Chronic head pain can quietly take over your mornings, your workdays, and your evenings, even when scans are “normal” and medications only help a little.
I am Dr. Alireza Chizari, and in this article I will walk you through how we think about care at a chronic headache clinic in Thousand Oaks and the surrounding area. My goal is to help you understand what is happening in your nervous system, how we evaluate chronic headaches in a precise and scientific way, and which non invasive treatments we can use to help you move toward steadier, clearer days.
Chronic Headache Clinic in Thousand Oaks for Lasting Relief
You are the hero of this story. You are the one who has pushed through meetings, family responsibilities, and sleepless nights despite pain that other people cannot see. My role, and the role of our team at California Brain & Spine Center in Calabasas, is to act as your expert guide and partner.
If you are searching for a chronic headache clinic in Thousand Oaks that respects your experience, uses advanced neurological tools, and focuses on safe, non invasive care, this page will show you exactly how we can help and what your next step can be.

Why chronic headaches in Thousand Oaks deserve serious attention
Many people are told their headaches are “just stress” or “just tension” and are sent home with stronger painkillers. Yet chronic daily headaches are one of the most disabling neurological problems worldwide. Chronic headache is often defined as headache on 15 or more days per month for at least 3 months.
That pattern changes everything. It is no longer an occasional inconvenience. It affects:
-
How reliable you feel at work
-
How present you can be with your family
-
How confident you feel making plans
From my perspective as someone trained in Electrical Engineering, Advanced Engineering & Management, and later Clinical Neuroscience, your headache pattern is data. It reflects how different networks in your brain, neck, autonomic nervous system, and sometimes vestibular system are interacting over time.
When I sit with a patient from Thousand Oaks who has lived with chronic headaches, I am not only listening for the “type” of headache, such as migraine or tension type. I am listening for:
-
Changes in the pattern over the years
-
Links to previous concussions, whiplash, or neck injuries
-
Sleep disruption, brain fog, dizziness, or memory problems
-
Medication overuse, where painkillers themselves start to keep the cycle going
A chronic headache clinic in Thousand Oaks has to do more than name your pain. It has to understand the system behind it.
Chronic headaches rarely exist in isolation. Many of our patients quietly deal with motion triggered dizziness, brain fog, or feeling “spaced out” when they walk through supermarkets or scroll on their phone. These signs often point to a vestibular or brainstem component that has not been fully addressed. If you recognize yourself in that picture, our article on migraine dizziness specialist in Westlake Village shows how we look beyond pain scores to uncover hidden balance and eye movement problems that may be fueling your headaches.

When a chronic headache clinic in Thousand Oaks is the right next step
You might ask yourself, “Is this really bad enough to see a specialist?” That doubt keeps many people stuck for years. In reality, getting an expert evaluation earlier can often prevent headaches from becoming more entrenched.
A specialized chronic headache clinic in Thousand Oaks or nearby is usually the right step if:
-
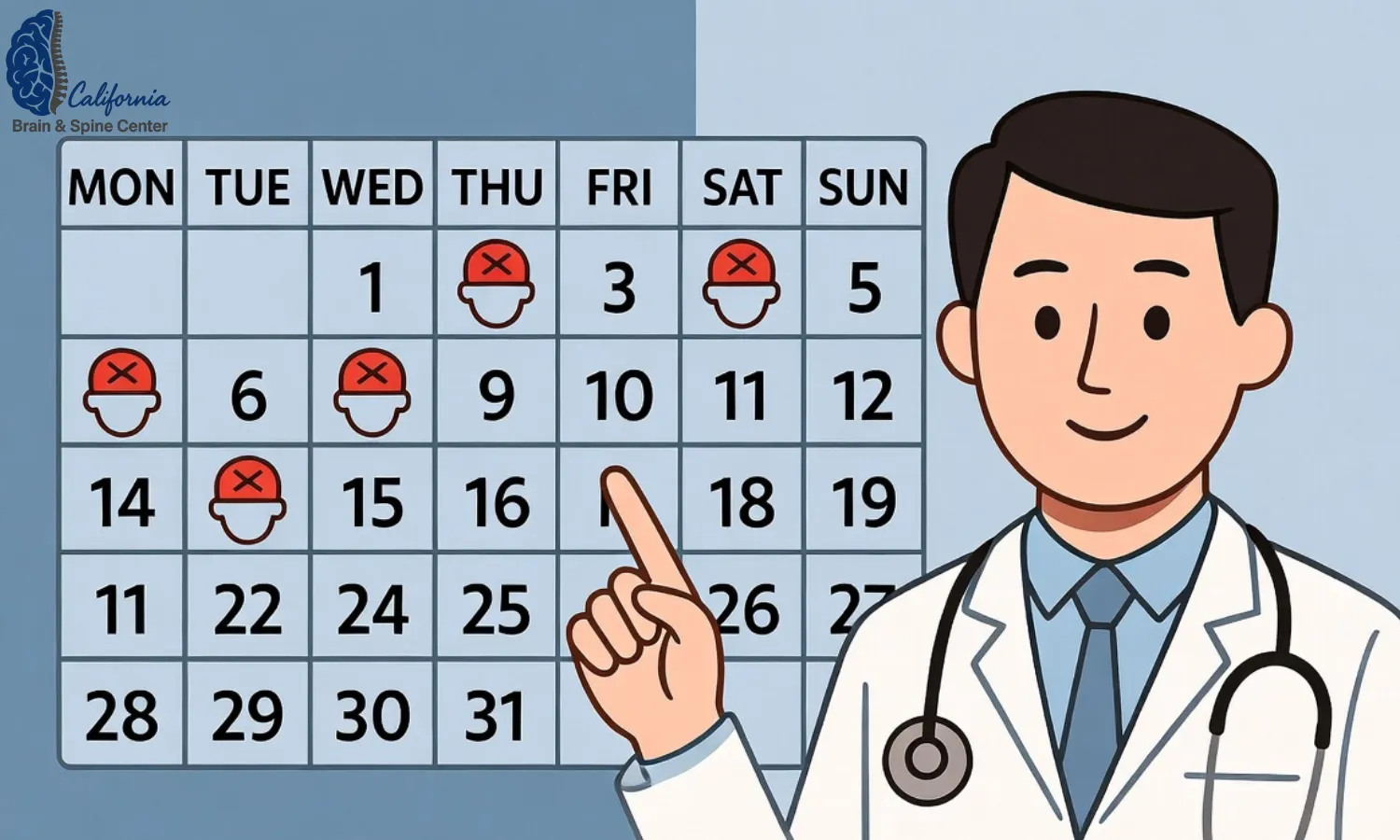
You have headaches on 15 or more days per month for longer than 3 months
-
Your headaches are getting more frequent, more intense, or more unpredictable
-
Over the counter medications are needed more than a few days per week, or you worry about relying on them
-
Headaches now come with dizziness, visual changes, brain fog, nausea, or balance problems
-
You have a history of concussion, head trauma, or whiplash and your headaches never fully settled
There are also red flag symptoms that always require urgent medical evaluation before any clinic focuses on “chronic headache”:
-
Sudden, severe “thunderclap” headache
-
Headache with weakness, vision loss, trouble speaking, or confusion
-
New headache with fever, stiff neck, or rash
-
New or different headache after age 50
If these are present, emergency care comes first. A responsible chronic headache clinic will always screen for these before designing any long term plan.
You are not “too sensitive” because you seek help for daily pain. You are simply listening to a body that has been asking for a different kind of attention for a long time.
Inside a chronic headache clinic in Thousand Oaks – how the team thinks
At California Brain & Spine Center, patients who look for a chronic headache clinic in Thousand Oaks are seen in the Calabasas office, a short drive away. The clinic serves Thousand Oaks, Westlake Village, Agoura Hills, Woodland Hills, Malibu, and the wider Southern California region.
Rather than treating headaches as a single symptom, the team thinks in terms of systems:
-
Brain networks involved in pain, vision, and sensory processing
-
Cervical spine and musculoskeletal function
-
Vestibular and balance systems
-
Autonomic regulation of heart rate, blood pressure, and stress responses
This integrated view reflects Dr. Chizari’s engineering background and his postdoctoral training in Clinical Neuroscience. It also supports the principles of neuroplasticity rehabilitation, where the brain can change its patterns in response to targeted input.
Step 1 – A structured neurological and headache history
At the first visit, patients are guided through a detailed history that explores:
-
Headache onset, frequency, duration, and character
-
Associated symptoms such as nausea, sensitivity to light or sound, aura, dizziness, or cognitive changes, all aligned with accepted migraine and chronic headache criteria
-
Medication use, including over the counter painkillers, triptans, or preventive drugs
-
Past injuries, especially concussion, whiplash, or spinal issues
-
Sleep, stress, hormonal patterns, and lifestyle triggers
This is not a quick “yes or no” checklist. It is a structured conversation that looks for patterns over years, not just days.
Step 2 – Focused examination and red flag screening
A complete neurological and musculoskeletal examination is then performed. This includes:
-
Cranial nerve and sensory testing
-
Muscle strength and coordination
-
Assessment of neck mobility, posture, and muscular tension
-
Screening for signs that might suggest a secondary cause of headache, such as neurological deficits or papilledema
The goal is to identify whether chronic headaches are likely to be primary (such as chronic migraine or chronic tension type headache) or whether there is any evidence of an underlying structural, vascular, or inflammatory condition that needs medical imaging or referral.
Step 3 – Advanced functional and vestibular assessment
For many chronic headache patients, especially those who also report dizziness, imbalance, or visual strain, functional testing is added:
-
Vestibular and balance testing
-
Eye movement and visual tracking evaluation
-
Gait and postural control assessment
-
Autonomic markers such as heart rate changes with position, when dysautonomia is suspected
This is where the clinic’s focus on dizziness, balance disorders, and autonomic nervous system disorders becomes directly relevant to chronic headache care.
A precise diagnosis is not just a label. It is a map that tells you which roads are worth walking and which ones are dead ends.

Non invasive treatment options for chronic headaches in Thousand Oaks
Once the pattern of headache and nervous system function is clear, treatment is planned in a personalized and layered way. At California Brain & Spine Center, chronic headache care for patients from Thousand Oaks often combines structural, neurological, and neuromodulation based approaches.
Neuroplasticity driven structural care
For patients whose chronic headaches are linked to neck tension, past whiplash, or postural overload, structural care is often part of the plan. Using the precise Gonstead chiropractic technique, the clinician focuses on specific spinal segments rather than broad, generalized manipulation.
The aim is to:
-
Reduce mechanical irritation and muscular guarding in the cervical spine
-
Improve joint motion and alignment that may be contributing to tension type or cervicogenic headaches
-
Support healthier input from the neck into the brainstem, where many headache pathways converge
This work is performed gently and in a graded fashion, always integrated with the overall neurological picture.
Vestibular rehabilitation and NeuroSensory Integration
For patients whose chronic headaches are entangled with dizziness, visual motion sensitivity, or past concussion, vestibular rehabilitation and NeuroSensory Integration (NSI) play an important role. Vestibular rehabilitation is a specialized form of physical therapy that uses exercises to retrain the brain’s response to motion and head position.
NSI expands on this by addressing:
-
Visual tracking and eye head coordination
-
Balance and spatial orientation
-
Integration between visual, vestibular, and proprioceptive inputs
By improving how these systems work together, the clinic aims to reduce the sensory overload that can trigger or amplify chronic headaches.
Cognitive and autonomic support
For some patients, chronic headache is tied to cognitive fatigue, brain fog, and autonomic instability such as heart rate swings or orthostatic intolerance. In these cases, elements of cognitive rehabilitation and autonomic retraining may be added, focusing on:
-
Attention, processing speed, and pacing strategies
-
Gentle graded activity to support autonomic resilience
-
Breathing and relaxation techniques to reduce sympathetic overdrive
Healing the brain is not about doing more. It is about doing the right things, in the right sequence, at the right intensity for your nervous system.

Neuromodulation – LLLT, PEMF, HBOT, GammaCore, and the NeuroRevive Program
In selected cases, the chronic headache clinic model for Thousand Oaks patients also includes non invasive neuromodulation technologies. These are used to support neuroplasticity and pain modulation, not as stand alone “magic bullets.”
Options may include:
-
Low-Level Laser Therapy (LLLT) to influence local blood flow and cellular activity in targeted regions
-
Pulsed Electromagnetic Field (PEMF) therapy to modulate cellular signaling and inflammation
-
Hyperbaric Oxygen Therapy (HBOT) to increase oxygenation of sensitive brain regions and support recovery in patients with headache linked to traumatic brain injury
-
GammaCore vagus nerve stimulation to help regulate pain pathways and autonomic tone
-
The NeuroRevive Program, which combines specific neuromodulation tools with tailored exercises and cognitive strategies
These tools are always integrated into a broader plan that includes careful headache classification, lifestyle guidance, and collaboration with the patient’s neurologist or primary care physician when medication decisions are involved.
Technology should never replace listening. It should amplify what is possible once we truly understand your story.

Lifestyle, medication overuse, and simple changes that protect your brain
For chronic headache, there is strong evidence that simple lifestyle patterns can either worsen or support your condition, especially when combined with professional care. Guidelines on headache management consistently emphasize sleep, hydration, exercise, and avoiding medication overuse.
A chronic headache clinic in Thousand Oaks that aims for long term results will usually help patients:
-
Build more regular sleep and wake cycles
-
Reduce reliance on frequent short acting painkillers to lower the risk of medication overuse headache
-
Track triggers such as skipped meals, dehydration, caffeine swings, and high screen time
-
Incorporate gentle, regular physical activity rather than sporadic intense workouts
These are not “one size fits all” rules. They are levers that can be adjusted to fit your reality, work schedule, and family life.
How long does a chronic headache program take for Thousand Oaks patients
The timeline for improvement is different for each person. However, many patients experience stages:
-
Stabilization – Reducing the frequency of the worst attacks and creating a safer pattern of medication use.
-
Recalibration – Using neurological, vestibular, structural, and neuromodulation tools to change how the brain processes pain and sensory input.
-
Resilience – Strengthening systems so that stress, travel, hormonal shifts, or minor illnesses are less likely to trigger severe flares.
Chronic headaches often develop over years. It is realistic to expect that meaningful, stable change takes time. The advantage of a structured approach is that you are not guessing or trying random things. Each step has a clear rationale based on headache science and clinical experience.
Progress with chronic pain rarely looks like a straight line. It looks like learning to bend without breaking, and noticing that over time the bad days lose their grip on your life.
Living with daily or near daily headaches changes how you work, socialize, and even plan your day. Simply rotating through medications without understanding the neurological “why” keeps many patients stuck. In our care for chronic neurological pain, we use targeted brain based treatments, neuromodulation, and lifestyle guidance to calm sensitized pain pathways instead of masking them, helping patients in Thousand Oaks and the surrounding area reclaim control over their life.
A real story from a Thousand Oaks patient with chronic headaches
Let me bring this back to first person, because stories often make the possibilities more real.
Some time ago, a patient in his early 50s from Thousand Oaks came to see me after almost 10 years of chronic headaches. He described a constant “pressure band” around his head most days of the month, with regular spikes that forced him to lie down in a dark room. He was still working, but he felt like his world had shrunk to work, pain, and recovery.
He had tried multiple medications. Some helped for a while, but he started needing them more and more often. Whenever he attempted to reduce them, his headaches would seem to rebound. He also had a history of a significant whiplash injury from a car accident many years earlier, which had never been treated in a targeted way.
At our first visit, we approached his case as a chronic daily headache pattern, likely overlapping with chronic migraine and medication overuse. We performed a detailed neurological exam, cervical spine assessment, and vestibular and balance testing. There were no red flags that required emergency imaging, but there were clear signs of neck dysfunction, visual strain, and autonomic sensitivity.
His plan included:
-
Gradual restructuring of medication use in collaboration with his prescribing physician
-
Specific Gonstead based structural work to address cervical restrictions
-
Vestibular and NeuroSensory Integration exercises to reduce visual and motion related triggers
-
Short, carefully dosed neuromodulation sessions within the NeuroRevive framework
The first month was about trust and stabilization. By the third month, his “worst” headache days were less frequent and less intense. By around six months, he reported more headache free days in a month than he had experienced in years. He was not “perfect,” but he had space again in his life to think about more than just pain.
He told me, “For the first time, I do not wake up automatically scanning for pain. I actually plan my day based on what I want to do.”
No two cases are identical, and I never promise specific outcomes. But this is an example of what can happen when we treat you as a whole person, guided by both science and story, instead of chasing isolated symptoms.
Your most common questions about chronic headache clinic in Thousand Oaks
Q1: How do I know if I really need a chronic headache clinic in Thousand Oaks or if I should just see my primary care doctor?
If your headaches are infrequent, mild, and respond well to simple measures, starting with a primary care doctor is reasonable. However, if you have headaches on 15 or more days per month, if they are getting worse, or if they are accompanied by dizziness, visual changes, or cognitive issues, specialized evaluation is often helpful. A chronic headache clinic in Thousand Oaks or nearby brings together neurological, structural, vestibular, and autonomic perspectives that go beyond routine care.
Q2: Will you change my medications or stop them?
Medication decisions are always made together with your prescribing physician or neurologist. At our clinic, we focus on understanding whether medication overuse might be part of your pattern and on adding non pharmacological tools, such as vestibular rehab, NeuroSensory Integration, and neuromodulation. In many cases, as your headaches become more stable, your medical team may choose to adjust medications, but this is done gradually and safely.
Q3: Are the treatments you use painful or invasive?
The core of our approach is non invasive. Structural care uses precise, controlled adjustments and soft tissue techniques. Vestibular and NSI exercises are usually gentle and tailored to your tolerance. Neuromodulation tools like LLLT, PEMF, HBOT, and GammaCore are designed to influence the nervous system without surgery or injections. You may feel challenged at times, but treatment should not feel like punishment.
Q4: How often would I need to come to the clinic from Thousand Oaks?
This depends on the severity and complexity of your case. Many patients start with more frequent visits during the initial stabilization and recalibration phase, then gradually reduce visit frequency as they gain resilience and learn home strategies. Because we are in Calabasas, the drive from Thousand Oaks is usually manageable, and some elements of follow up can occasionally be supported by telehealth when appropriate.
Q5: Can you help if my headaches started after a concussion or car accident?
Yes. A significant portion of our work involves post concussion and traumatic brain injury recovery. Chronic headaches after concussion often coexist with dizziness, balance issues, cognitive fatigue, and autonomic changes. In those cases, we integrate concussion treatment principles, vestibular rehabilitation, neuroplasticity rehabilitation, and sometimes HBOT or other neuromodulation tools within the NeuroRevive Program.
Q6: What is the first step if I am interested in your chronic headache clinic near Thousand Oaks?
The first step is a comprehensive evaluation. This includes a detailed history, targeted examination, and any appropriate functional testing. From there, we decide together whether our approach fits your needs and how a plan can be tailored to your goals and current capacity.
Conclusion – your next step toward clearer, calmer days
Chronic headaches can make life feel small and unpredictable, especially when you have already tried many things. In this article, I have walked you through how we approach care at a chronic headache clinic in Thousand Oaks and the surrounding communities.
We start by listening to your story and classifying your headache pattern using established criteria. We then look at your brain, neck, balance, and autonomic function as one connected system. From there, we design a personalized plan that may include precise structural care, vestibular rehabilitation, NeuroSensory Integration, cognitive support, and non invasive neuromodulation tools such as LLLT, PEMF, HBOT, GammaCore, and the NeuroRevive Program.
Most importantly, we never forget that you are the hero of this process. My background in engineering and clinical neuroscience allows me to bring technical precision to your case, but your goals and your lived experience drive our decisions.
If you are looking for a chronic headache clinic in Thousand Oaks that will take your pain seriously, respect your time, and work with you as a partner, I would be honored to meet you, learn your story, and see how we can help.
At the end of the day, the goal is not only fewer headaches. The goal is a life with more clarity, more freedom to plan, and more space for the people and activities that matter most to you.
If you recognize yourself in these descriptions and you live in or near Thousand Oaks, you do not have to keep pushing through chronic head pain alone. You can contact California Brain & Spine Center in Calabasas to schedule a personalized neurological and headache evaluation, ask your questions, and explore whether our approach is the right fit.
We are here to help you move toward the best version of your life and function, not just to temporarily quiet symptoms.
👨⚕️ Alireza Chizari, MSc, DC, DACNB
🧠 Clinical Focus
🔬 Assessment & Treatment Approach
Objective testing may include:
Treatment programs may involve:
📍 Clinic Information
✅ Medical Review
⚠️ Disclaimer
Comments
FAQ
What is Functional Neurology?
Functional Neurology is a healthcare specialty that focuses on assessing and rehabilitating the nervous system’s function. It emphasizes neuroplasticity—the brain’s ability to adapt and reorganize—using non-invasive, evidence-based interventions to improve neurological performance.
How does Functional Neurology differ from traditional neurology?
Traditional neurology often concentrates on diagnosing and treating neurological diseases through medications or surgery. In contrast, Functional Neurology aims to optimize the nervous system’s function by identifying and addressing dysfunctions through personalized, non-pharmaceutical interventions.
Is Functional Neurology a replacement for traditional medical care?
No. Functional Neurology is intended to complement, not replace, traditional medical care. Practitioners often collaborate with medical professionals to provide comprehensive care.
What conditions can Functional Neurology help manage?
Functional Neurology has been applied to various conditions, including:
• Concussions and Post-Concussion Syndrome
• Traumatic Brain Injuries (TBI)
• Vestibular Disorders
• Migraines and Headaches
• Neurodevelopmental Disorders (e.g., ADHD, Autism)
• Movement Disorders
• Dysautonomia
• Peripheral Neuropathy
• Functional Neurological Disorder (FND)
Can Functional Neurology assist with neurodegenerative diseases?
While Functional Neurology does not cure neurodegenerative diseases, it can help manage symptoms and improve quality of life by optimizing the function of existing neural pathways.
What diagnostic methods are used in Functional Neurology?
Functional Neurologists employ various assessments, including:
• Videonystagmography (VNG)
• Computerized Posturography
• Oculomotor Testing
• Vestibular Function Tests
• Neurocognitive Evaluations
How is a patient’s progress monitored?
Progress is tracked through repeated assessments, patient-reported outcomes, and objective measures such as balance tests, eye movement tracking, and cognitive performance evaluations.
What therapies are commonly used in Functional Neurology?
Interventions may include:
- Vestibular Rehabilitation
- Oculomotor Exercises
- Sensorimotor Integration
- Cognitive Training
- Balance and Coordination Exercises
- Nutritional Counseling
- Lifestyle Modifications
Are these therapies personalized?
Absolutely. Treatment plans are tailored to the individual’s specific neurological findings, symptoms, and functional goals.
Who can benefit from Functional Neurology?
Individuals with unresolved neurological symptoms, those seeking non-pharmaceutical interventions, or patients aiming to optimize brain function can benefit from Functional Neurology.
Is Functional Neurology suitable for children?
Yes. Children with developmental delays, learning difficulties, or neurodevelopmental disorders may benefit from Functional Neurology approaches.
How does Functional Neurology complement other medical treatments?
It can serve as an adjunct to traditional medical care, enhancing outcomes by addressing functional aspects of the nervous system that may not be targeted by conventional treatments.
How is technology integrated into Functional Neurology?
Technological tools such as virtual reality, neurofeedback, and advanced diagnostic equipment are increasingly used to assess and enhance neurological function.
What is the role of research in Functional Neurology?
Ongoing research continues to refine assessment techniques, therapeutic interventions, and our understanding of neuroplasticity, contributing to the evolution of Functional Neurology practices.

Dr. Alireza Chizari
Latest articles
